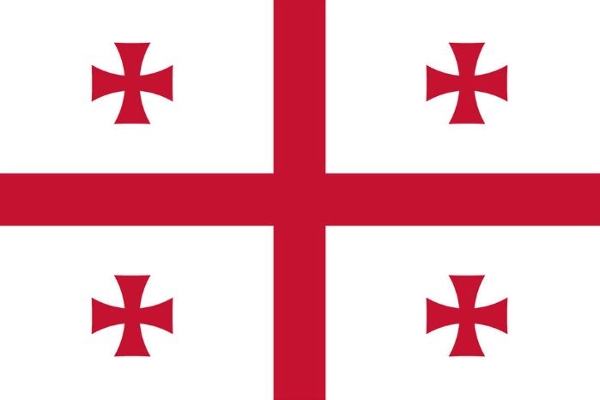
Georgia
Institutions
The National Center for Tuberculosis and Lung Diseases
The National Center for TB and Lung Diseases (NCTLD) reports to the Georgian Ministry of Health and NCTLD leaders strongly support the ongoing collaborative activities in the area of TB research and training. The NCTLD has collaborated with Emory University since the initial NIH funding of the Emory Global TB Research Training Program in 2004. The NCTLD is responsible for TB treatment and treatment guidelines in Georgia, manages TB drug procurement as well as the drug resistant TB (MDR- and XDR-TB) treatment program in Georgia, and has ongoing funding and a well-established research infrastructure. The NCTLD is actively participating in three anti-TB drug development clinical trials, one phase 2 trial (SimpliciTB) and four phase 3 trials (Zenix TB, STREAM 2 and two Horizon 2020 trials). NCTLD is also the recipient of a 5-year grant totaling 21 million Euros from the Global Fund to Fight AIDS, TB, and Malaria.
